Depression
What Is Depression: Causes, Symptoms, Diagnosis, Treatment
What is depression?

What are the causes of depression?
- Genetic predisposition: Individuals with a family history of depression have a higher risk of developing this disorder.
- Neurochemical imbalances: Changes in neurotransmitter levels, such as serotonin and dopamine, can contribute to the onset of depression.
- Traumatic events: Traumatic experiences, such as the loss of a loved one or highly stressful life events, can trigger depression.
- Chronic stress: Long-term stressful situations at work or in personal life can contribute to the development of depression.
- Hormonal issues: Hormonal imbalances, such as those related to pregnancy or menopause, can influence mood.
How many types of depression are there?
There are several types of depression, each with distinct characteristics and requiring specific treatment approaches.
Below are the main subtypes of depression, along with concrete examples for each:
Major depression is characterized by a deep and persistent state of sadness, loss of interest in daily activities, and multiple physical and emotional symptoms lasting at least two weeks.
Example:
Maria, a 45-year-old teacher, is struggling with major depression. For several weeks, she has felt overwhelmed by sadness, no longer finds pleasure in teaching her students, and has significant difficulty getting out of bed in the morning. In addition, she has begun to lose weight and experience sleep problems.
Dysthymia is a chronic form of depression with milder symptoms than major depression, but it lasts much longer—often for years.
Example:
Mihai, a 38-year-old engineer, has been struggling with dysthymia for over five years. Although he is able to function at work, he constantly feels low in energy and enthusiasm. He has a persistent sad mood and has lost interest in former hobbies, such as hiking.
Bipolar disorder involves depressive episodes that alternate with episodes of mania or hypomania. The depressive phases are similar to major depression.
Example:
Cristina, aged 29, has been diagnosed with bipolar disorder. During depressive episodes, she feels extremely tired and hopeless. These periods are followed by manic episodes in which she has excessive energy, speaks rapidly, and makes impulsive decisions, such as uncontrolled spending.
Postpartum depression occurs after childbirth and is characterized by severe depressive symptoms, anxiety, and exhaustion that make caring for the newborn and managing daily responsibilities difficult.
Example:
Ana, a 32-year-old mother, experiences postpartum depression a few weeks after the birth of her first child. She feels overwhelmed, cries frequently, and has feelings of worthlessness. She also finds it difficult to bond with her baby and feels guilty for not being able to be a “good mother.”
Seasonal depression is a form of depression that occurs regularly during certain times of the year, usually in autumn and winter, when daylight hours are shorter and natural light is reduced.
Example:
Paul, a 22-year-old student, suffers from seasonal depression. Every winter, he experiences a significant drop in energy, difficulty concentrating, and a constant desire to sleep. His mood improves considerably in spring and summer.
Psychotic depression is a severe form of major depression accompanied by psychotic symptoms, such as hallucinations or delusions.
Example:
Irina, a 40-year-old woman, has been diagnosed with psychotic depression. In addition to severe depressive symptoms such as loss of interest in life and feelings of worthlessness, she experiences auditory hallucinations and believes she is being followed by people who want to harm her.
Atypical depression is a subtype of major depression characterized by a specific pattern of symptoms, including mood reactivity to positive events, weight gain, excessive sleep, a heavy feeling in the arms and legs, and sensitivity to rejection.
Example:
Elena, a 35-year-old accountant, suffers from atypical depression. Although she often feels depressed and fatigued, she notices a temporary improvement in mood when she receives good news or spends time with friends. She tends to overeat, sleep more than usual, and frequently feels rejected by others.
What is the difference between depression and anxiety?
Although depression and anxiety are often discussed together and share many similar symptoms, causes, and treatment approaches, they are two distinct mental health conditions.
There are, however, several key differences. People with depression tend to move more slowly, and their reactions may appear flattened or blunted. Individuals with anxiety, on the other hand, tend to be hypervigilant, as they struggle to manage intrusive and debilitating internal thoughts.
Another important distinction is the presence of fear related to the future in people with anxiety. Individuals with depression who do not also experience anxiety are less likely to worry excessively about future events, as they are often resigned to the belief that things will continue to be bad regardless of what happens. In other words, they tend to predict the future based on how they feel in the present moment.
What risk factors can lead to depression?
Depression is a complex mental health disorder influenced by a combination of genetic, biological, environmental, and psychological factors. Identifying risk factors is essential for better understanding the condition and for developing effective prevention and treatment strategies.
The main risk factors for depression include:
Genetic and hereditary factors
A family history of depression can increase the risk of developing this disorder. Genetic studies have shown that individuals with first-degree relatives (parents or siblings) who suffer from depression are at a higher risk of experiencing depressive symptoms. According to a study published in the Journal of Affective Disorders, the risk of depression is two to three times higher in individuals with a family history of major depression.
Biological factors
Imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine are associated with depression. These chemicals play a crucial role in regulating mood and emotions. Research published in Nature Reviews Neuroscience highlights the importance of neurotransmitters in the pathogenesis of depression and the effectiveness of antidepressant treatments.
Chronic inflammation has also been linked to depression. Inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) are often elevated in individuals with depression. A study published in Molecular Psychiatry showed that systemic inflammation may contribute to the development and persistence of depressive symptoms.
Environmental factors
Traumatic experiences, such as physical or emotional abuse, the loss of a loved one, divorce, or financial difficulties, can trigger depressive episodes. According to a longitudinal study published in the Journal of Affective Disorders, individuals who experience stressful life events have a significantly higher risk of developing depression.
Social isolation and lack of emotional support can worsen depressive symptoms. A strong and supportive social network can act as a protective factor against depression.
Psychological factors
Certain personality traits, such as perfectionism, low self-esteem, and a tendency toward excessive negative thinking, can increase vulnerability to depression. A study published in the Journal of Personality found that neurotic personality traits are strongly associated with an increased risk of depression.
Chronic stress—whether related to work or daily responsibilities—can lead to emotional exhaustion and the onset of depression. Research published in Psychological Bulletin emphasizes that chronic stress and ineffective coping mechanisms are major risk factors for developing depression.
Lifestyle-related factors
Physical inactivity and a sedentary lifestyle are associated with an increased risk of depression. Regular physical activity can improve mood and reduce depressive symptoms. A study published in Medicine & Science in Sports & Exercise found that regular exercise is effective in preventing and treating depressive symptoms.
An unhealthy diet high in sugar and unhealthy fats may also contribute to depression. Essential nutrients such as omega-3 fatty acids, B vitamins, and magnesium play an important role in mental health. Research published in Public Health Nutrition shows that a healthy diet is associated with a lower risk of depression.
Who is at risk of developing depression?
- Individuals with a family history of depression
- Women
- Individuals with a history of traumatic events
- People with other mental health disorders
- Adolescents and young adults
- Individuals with chronic illnesses
- Socially isolated individuals
- People who consume alcohol or drugs

Women are twice as likely as men to experience depression. This difference may be explained by hormonal fluctuations related to menstruation, pregnancy, menopause, and the postpartum period, as well as gender-specific social and stress-related factors.
Those who have experienced trauma—such as physical or emotional abuse, the death of a loved one, divorce, or war-related experiences—are more likely to develop depression. These events can trigger severe emotional responses that contribute to depressive symptoms.
People with anxiety disorders, bipolar disorder, post-traumatic stress disorder (PTSD), or eating disorders have an increased risk of developing depression. These conditions can interact and exacerbate depressive symptoms.
Adolescents and young adults are particularly vulnerable due to hormonal changes, academic and social pressure, and major life transitions. The incidence of depression is increasing in this age group.
People suffering from chronic conditions such as diabetes, cardiovascular disease, cancer, or autoimmune disorders are more susceptible to depression. Persistent pain and physical limitations can contribute to feelings of sadness and hopelessness.
Those with limited social networks or insufficient emotional support are more prone to depression. Isolation and loneliness can intensify feelings of worthlessness and sadness.
Alcohol and drug use can increase the risk of depression by altering brain chemistry and worsening depressive symptoms.
What are the symptoms of depression?
Depression manifests itself through a variety of symptoms that can vary in severity and duration from one person to another. These symptoms affect a person’s emotional state as well as their physical and social functioning.
- Here are the main symptoms of depression and a detailed explanation for each:
- Persistent feelings of sadness and anxiety: People who suffer from depression often feel sad or anxious without an obvious cause. These feelings are persistent and do not go away on their own, affecting the ability to enjoy life.
- Loss of interest or pleasure in daily activities: A common symptom of depression is anhedonia, which refers to the loss of interest or pleasure in activities that were previously considered enjoyable, such as hobbies, sports, or socializing.
- Changes in appetite and weight: Depression can cause significant changes in appetite and weight. Some people may lose their appetite and lose weight, while others may experience an increased appetite and gain weight. These changes are unintentional and are linked to emotional state.
- Sleep problems: Sleep disturbances are common in people with depression. These may include insomnia (difficulty falling asleep or staying asleep), hypersomnia (excessive sleep), or frequent awakenings during the night. Poor-quality sleep contributes to the worsening of depressive symptoms.
- Lack of energy or constant fatigue: People with depression often feel exhausted and lacking in energy, even after a night of adequate sleep. This constant fatigue affects the ability to carry out daily tasks and function normally.
- Feelings of worthlessness or guilt: Depression can cause intense feelings of worthlessness, guilt, or self-blame. Affected individuals may feel that they are useless or that they have failed in life, even when there are no real reasons for these feelings.
- Difficulties with concentration, decision-making, or memory: Cognitive problems are common in depression. These include difficulties concentrating, problems making decisions, and memory issues. These symptoms can affect academic or professional performance and contribute to feelings of inadequacy.


How does depression manifest in children and adolescents?
Depression can also affect children and adolescents, often manifesting differently than in adults. It is important to recognize the symptoms specific to this age group in order to provide appropriate support and treatment.
Depression in children and adolescents may present as follows:
- Sadness and irritability: Persistent feelings of sadness or irritability without a clear reason.
- Lack of interest in activities: Loss of interest in previously enjoyable activities, withdrawal from school and social activities.
- Changes in appetite and weight: Weight changes due to decreased or increased appetite.
- Sleep problems: Difficulty falling asleep, excessive sleeping, or frequent awakenings.
- Fatigue and low energy: Constant tiredness and lack of energy.
- Irritability and anger outbursts: Increased irritability, temper tantrums, and exaggerated reactions to minor situations.
- Difficulty concentrating: Impaired concentration and attention, poor academic performance.
- Social withdrawal: Avoidance of social interactions and a preference for being alone.
- Physical complaints: Frequent complaints of physical pain without a clear medical cause.
- Risky behavior: Risk-taking behaviors such as alcohol and drug use, unprotected sexual activity, or self-harm.
How does depression manifest in adults?
Depression in adults is a complex condition that can profoundly affect both personal and professional life. Understanding how this illness manifests is essential in order to intervene in a timely manner.
Depression in adults may manifest as follows:
- Persistent sadness and loss of interest: Adults with depression may experience deep and persistent sadness that does not go away. This is often accompanied by a loss of interest in activities that once brought pleasure.
- Changes in appetite and weight: Depression can cause significant weight fluctuations, either through loss of appetite and weight loss or increased appetite and weight gain.
- Sleep problems: Adults with depression may experience severe insomnia, frequent nighttime awakenings, or hypersomnia, characterized by excessive and unrefreshing sleep.
- Fatigue and lack of energy: Persistent fatigue and low energy levels are common. Even simple daily activities may feel overwhelming.
- Difficulty concentrating: Depression affects concentration and memory, making decision-making and completing daily tasks difficult.
Social withdrawal: Depression can lead to withdrawal from social activities and avoidance of interactions with family and friends. Adults may become isolated and spend long periods alone.

What disorders are commonly associated with depression?
Depression is often accompanied by other mental health disorders, which can complicate diagnosis and treatment. Identifying and managing these comorbid conditions is essential for an effective therapeutic approach.
The most common disorders associated with depression include:
- Generalized Anxiety Disorder (GAD)
- Panic Disorder
- Obsessive-Compulsive Disorder (OCD)
- Eating Disorders
- Bipolar Disorder
- Borderline Personality Disorder (BPD)
- Sleep Disorders
Panic disorder involves recurrent and unexpected panic attacks accompanied by intense fear and physical symptoms such as palpitations and breathing difficulties. Depression may develop in individuals with panic disorder due to the negative impact of panic attacks on their lives. Constant fear of future panic attacks can also contribute to the onset of depression.
Obsessive-Compulsive Disorder is characterized by unwanted obsessive thoughts and repetitive compulsive behaviors performed to reduce the anxiety caused by these thoughts. The stress and frustration generated by OCD can lead to the development of depression. In addition, depressive symptoms may worsen compulsive behaviors.
Eating disorders such as anorexia and bulimia involve abnormal eating behaviors and excessive concern with weight and body image. Individuals with eating disorders often experience depressive symptoms due to negative self-evaluation and constant stress related to food and weight.
Bipolar disorder is characterized by alternating episodes of depression and episodes of mania or hypomania. Depressive episodes are a central component of bipolar disorder. Proper recognition and treatment of depressive episodes are crucial for managing this condition.
Borderline Personality Disorder is characterized by emotional instability, turbulent interpersonal relationships, an unstable self-image, and impulsive behaviors. Individuals with BPD often experience severe depressive episodes due to emotional instability and interpersonal difficulties.
Sleep disorders include insomnia, hypersomnia, and circadian rhythm disorders. These conditions can impair sleep quality and daily functioning. Depression is frequently associated with sleep disorders. Poor or insufficient sleep can worsen depressive symptoms, and conversely, depression can contribute to sleep problems.
How is depression diagnosed?
Diagnosing depression is a complex process that involves multiple steps to ensure a thorough and accurate evaluation of a person’s mental health.
The three main steps in the diagnostic process include:
Initial evaluation
The first step in diagnosing depression is often a visit to the primary care physician. The doctor will discuss the symptoms the patient is experiencing, as well as their duration and severity.
Psychiatric evaluation
If depression is suspected, the patient may be referred to a psychiatrist or clinical psychologist for a more detailed assessment. The specialist will conduct an in-depth clinical evaluation, discussing symptoms, life history, past trauma, and current stressors.
DSM-5 diagnostic criteria
Depression is often diagnosed based on criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).

According to the DSM-5, to be diagnosed with major depressive disorder, a patient must experience at least five of the following symptoms for a minimum of two weeks, with at least one of the symptoms being either depressed mood or loss of interest or pleasure:
- Depressed mood most of the day, nearly every day
- Markedly diminished interest or pleasure in all or almost all activities
- Significant weight loss or weight gain, or changes in appetite
- Insomnia or hypersomnia
- Psychomotor agitation or retardation
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or indecisiveness
- Recurrent thoughts of death or suicide
What treatment options are available for depression?
There are various treatment options for depression, tailored to the individual needs of each patient. The most commonly used approaches include medication, psychotherapy, alternative treatments, and lifestyle interventions.
The main treatment options include:
- Medication therapy
- Commonly used psychotherapies for depression
- Lifestyle interventions
- Antidepressants: Medications commonly used to treat depression.
- Adjunctive medications: In certain cases, adjunctive medications such as atypical antipsychotics or mood stabilizers may be prescribed to enhance the effectiveness of antidepressant treatment.
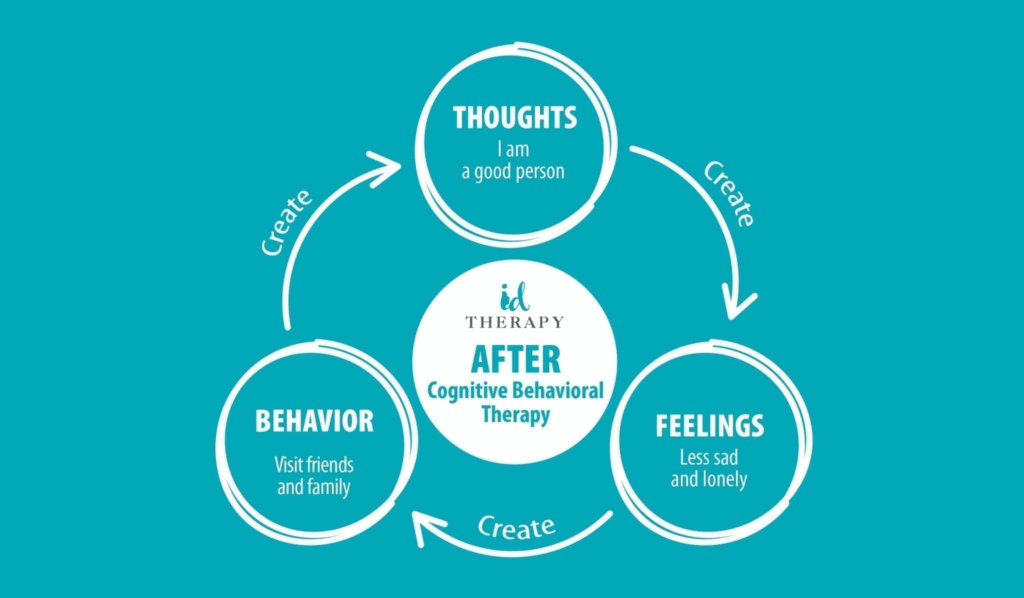
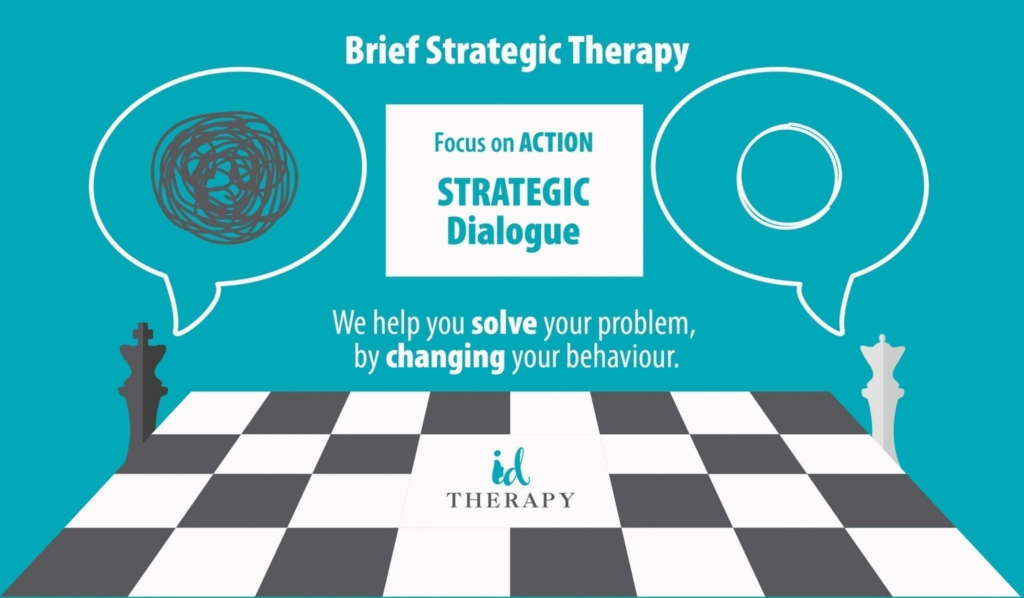
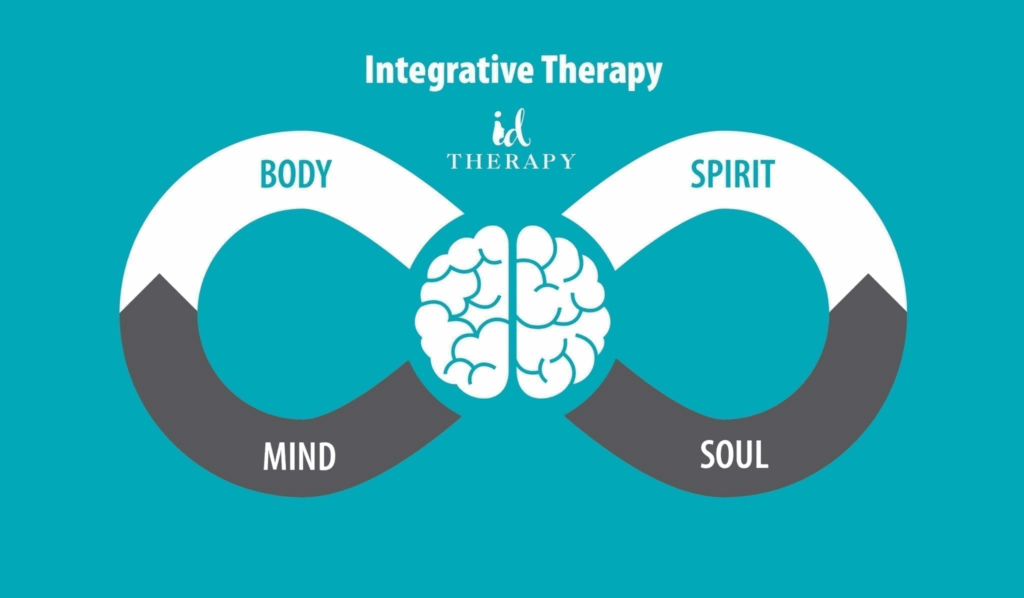
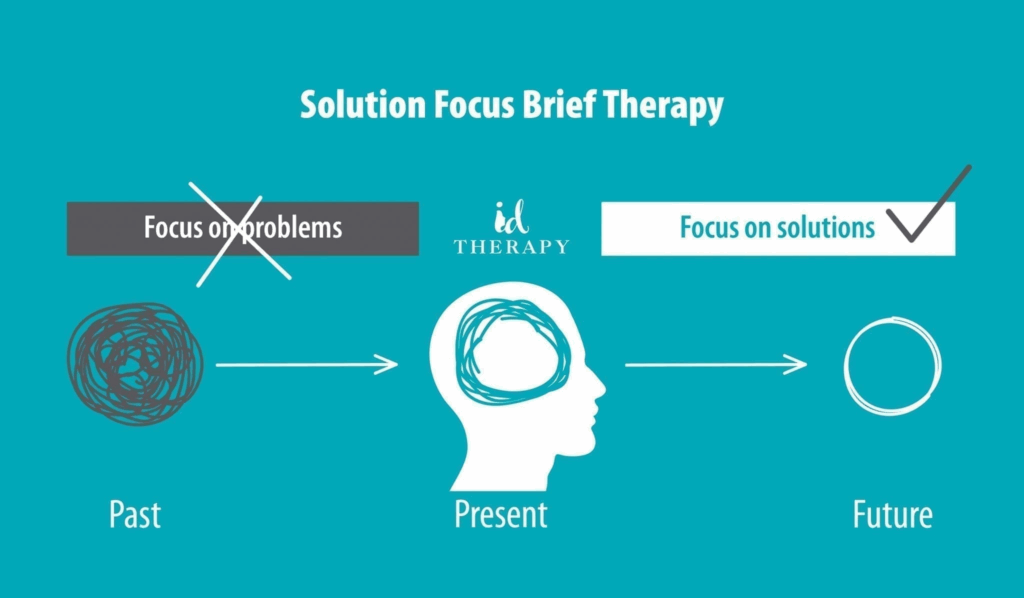
At ID Therapy Clinic, we combine different psychotherapeutic approaches to map the source and expression of each symptom.
We integrate therapeutic methods in an innovative way to simplify the path toward solutions and to diagnose symptoms within their broader context.
- Supplements and nutrition: Certain supplements such as omega-3 fatty acids, B and D vitamins, and magnesium may have beneficial effects on mental health.
- Acupuncture and meditation: Acupuncture and mindfulness meditation techniques can help reduce symptoms of depression and anxiety.
- Physical exercise: Regular physical activity can improve mood and energy levels while reducing depressive symptoms.
- Healthy nutrition: A balanced diet rich in essential nutrients supports mental health.
- Sleep regulation: Maintaining a regular sleep schedule and improving sleep quality are essential for managing depression.
- Assessment and diagnosis:ID Therapy offers comprehensive evaluations and accurate diagnoses for depression and other mental health disorders using modern and effective methods.
- Personalized psychotherapy:Specialists at ID Therapy provide personalized therapies, including Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT), and Psychodynamic Therapy, tailored to each patient’s needs.
- Couples and family therapy: ID Therapy also offers couples and family therapy to address relationship issues and to support family members in managing depression.

What Methods Exist to Prevent Depression?
Preventing depression involves adopting proactive measures and a healthy lifestyle to reduce the risk of developing this disorder.
Below are the most effective and commonly recommended methods for preventing depression:
- Maintaining Optimal Physical Health
Regular physical exercise and a balanced diet are essential in preventing depression. Aerobic physical activity stimulates the release of endorphins—chemicals that improve mood—while a diet rich in fruits, vegetables, lean proteins, and healthy fats supports mental health. Essential nutrients such as omega-3 fatty acids, B-complex vitamins, vitamin D, and magnesium play an important role in mood regulation and in preventing depressive symptoms.
- Effective Stress Management
Practicing relaxation techniques—such as meditation, yoga, and deep breathing—significantly contributes to reducing stress and preventing depression.
In addition, effective organization of daily activities, setting realistic goals, and proper time management help reduce feelings of overwhelm and maintain healthy emotional balance.
- Social Support
Maintaining positive and supportive relationships with family, friends, and colleagues provides essential emotional support. Engaging in social activities and staying connected with others helps prevent isolation and feelings of loneliness.
Participating in support groups or communities with shared interests fosters a sense of belonging and contributes to the development of effective coping strategies.
- Self-Awareness and Personal Development
Psychological counseling and therapy are useful not only for treating depression but also for preventing it. Working with a therapist helps identify risk factors, understand emotional patterns, and develop healthy coping mechanisms.
- Avoiding Substance Use
Alcohol and drug use can significantly increase the risk of depression. Limiting or avoiding these substances and seeking specialized help in cases of addiction are essential steps in preventing depression.
What Complications Can Occur If Depression Is Not Treated?
Untreated depression can have serious consequences on physical, mental, and emotional health, affecting all aspects of a person’s life.
- Worsening of Depressive Symptoms
Without treatment, depressive symptoms may become more severe and harder to manage. Deep sadness, lack of energy, feelings of worthlessness, and hopelessness may intensify, significantly reducing quality of life.
If untreated, depression can progress into a major depressive episode, characterized by severe symptoms lasting at least two weeks and severely interfering with daily functioning.
- Physical Health Problems
Depression is associated with an increased risk of cardiovascular diseases, including hypertension and heart attack. Chronic emotional stress and inflammation may contribute to the development of these conditions.
Additionally, depression can weaken the immune system, increasing vulnerability to infections and slowing recovery.
- Difficulties in Interpersonal Relationships
Untreated depression can lead to tension and conflict in close relationships. The affected individual may become irritable, withdrawn, or emotionally distant, negatively impacting relationships with family and friends.
- Social Isolation
Avoidance of social interactions is common in untreated depression. This isolation can worsen depressive symptoms and contribute to a vicious cycle of loneliness and emotional suffering.
- Financial and Professional Problems
Reduced work performance, absenteeism, or inability to work may lead to loss of income and financial difficulties. In addition, delayed medical treatment can result in higher healthcare costs.
How Can ID Therapy Clinic Help in Treating Depression?
ID Therapy is a clinic specialized in the treatment of depression and other mental health disorders, offering personalized services based on thorough evaluations and modern therapeutic methods.
The ID Therapy approach includes:
- Assessment and Diagnosis Comprehensive clinical evaluation, accurate diagnosis, and development of a personalized treatment plan.
- Personalized Psychotherapy Cognitive Behavioral Therapy and Integrative Therapy, tailored to each patient’s needs.
- Nurosym Advanced neuromodulation
Experience advanced neuromodulation
Free yourself from stress and anxiety – breathing exercises
Through this integrated approach, ID Therapy helps patients overcome depression and regain a healthy and balanced life.
Depression is a serious mental health issue that requires attention and appropriate treatment. Early identification of symptoms and seeking professional help are essential for preventing complications and improving quality of life.
ID Therapy Clinic is a specialized center that provides comprehensive and personalized solutions for the treatment of depression, combining medical expertise with holistic support to assist patients on their journey toward recovery. If you are experiencing symptoms of depression, do not hesitate to contact ID Therapy to receive the necessary help and begin the recovery process.
Adress: Naum Ramniceanu Street, no. 23, ap. 1, Sector 1, Bucharest, Romania
